The clinical documentation integrity practitioner (CDIP) performed a verbal query and then later neglected following up with the provider. How should the CDIP avoid a compliance risk for this follow up failure according to AHIMA's Guidelines for Achieving a Compliant Query Practice?
Correct Answer:
D
According to AHIMA??s Guidelines for Achieving a Compliant Query Practice, the clinical documentation integrity practitioner (CDIP) should complete the documentation at the time of discussion or immediately following to avoid a compliance risk for this follow up failure. This is because verbal queries are considered part of the health record and must be documented in a timely and accurate manner to reflect the provider??s response and any changes in documentation or coding. Completing the documentation later or only when there is an agreement may result in errors, omissions, inconsistencies, or delays that may affect the quality and integrity of the health record and the query process. (AHIMA Guidelines for Achieving a Compliant Query Practice1)
References:
✑ AHIMA Guidelines for Achieving a Compliant Query Practice1
Hospital policy states that physician responses to queries should be no longer than timely payer filing requirements. A physician responds to a query after the final bill has been submitted. How should administration respond in this situation?
Correct Answer:
B
Administration should respond to this situation by reviewing the record to determine any potential data integrity impact and/or rebilling implications. According to the AHIMA Practice Brief on Managing an Effective Query Process, post-bill queries are generally initiated as a result of an audit or other internal monitor, and healthcare entities can develop a policy regarding whether they will generate post-bill queries and the timeframe following claims generation that queries may be initiated. The practice brief also states that healthcare entities should consider the following three concepts in the development of a post-bill (including query) policy: applying normal course of business guidelines, using payer-specific rules on rebilling timeframes, and determining reliability of query response over time 2. Therefore, administration should review the record to see if the physician??s response to the query affects the quality of care, patient safety, severity of illness, risk of mortality, or reimbursement, and if so, whether it is appropriate and feasible to rebill the account based on the payer??s rules and the normal course of business guidelines. Administration should also evaluate the reasons for the physician??s delayed response and provide feedback and education to prevent future occurrences.
References: 1: AHIMA CDIP Exam Prep, Fourth Edition, p. 133 3 2: AHIMA Practice Brief: Managing an Effective Query Process 4
Which physician would best benefit from additional education for unanswered queries?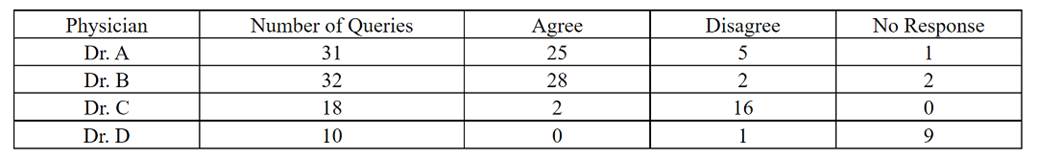
Correct Answer:
D
According to the Documentation Integrity Practitioner (CDIP®) study guide, the physician with the highest number of unanswered queries would benefit from additional education. In this case, Dr. D has the highest number of unanswered queries with 9. Unanswered queries may indicate a lack of understanding, engagement, or compliance with the query process, which may affect the quality and accuracy of clinical documentation and coding1. Therefore, Dr. D would best benefit from additional education for unanswered queries, such as the importance of timely and appropriate query responses, the impact of queries on severity of illness, risk of mortality, and reimbursement, and the best practices for a compliant query practice2. References:
✑ Q&A: What to do with unanswered queries | ACDIS
✑ Guidelines for Achieving a Compliant Query Practice (2019 Update) - AHIMA
Which of the following should be shared to ensure a clear sense of what clinical documentation integrity (CDI) is and the CDI practitioner's role within the organization?
Correct Answer:
D
Sharing the mission of the CDI program should be done to ensure a clear sense of what CDI is and the CDI practitioner??s role within the organization. The mission statement defines the purpose, goals, and values of the CDI program, and how it aligns with the organization??s vision and strategy. The mission statement also communicates the benefits and expectations of the CDI program to various stakeholders, such as providers, executives, coders, quality staff, and patients. The mission statement can help establish the credibility, professionalism, and identity of the CDI practitioners, and guide their daily activities and decisions 2.
References: 1: AHIMA CDIP Exam Prep, Fourth Edition, p. 133 3 2: Mission CDI: Guiding goals, values, and principles 1
A clinical documentation integrity practitioner (CDIP) is reviewing an outpatient surgical chart. The patient underwent a laparoscopic appendectomy for acute gangrenous appendicitis. Which coding reference should be used for coding advice on correct assignment of the procedure code for proper ambulatory payment classification (APC) reimbursement?
Correct Answer:
C
The coding reference that should be used for coding advice on correct assignment of the procedure code for proper ambulatory payment classification (APC) reimbursement is the AMA CPT Assistant. The CPT Assistant is the official source of guidance from the American Medical Association (AMA) on the proper use and interpretation of the Current Procedural Terminology (CPT) codes, which are used to report outpatient and professional services. The CPT Assistant provides clinical scenarios, frequently asked questions, coding tips, and updates on CPT coding changes. The CPT codes are used to determine the APC reimbursement for outpatient services under the Medicare Outpatient Prospective Payment System (OPPS). (CDIP Exam Preparation Guide)
References:
✑ CDIP Exam Content Outline1
✑ CDIP Exam Preparation Guide2
✑ AMA CPT Assistant3
✑ Medicare Claims Processing Manual Chapter 4 - Part B Hospital (Including Inpatient Hospital Part B and OPPS)

